Abstract
Introduction
This is a radiographic study of ankylosing spondylitis patients with severe fixed kyphotic deformity who underwent pedicle subtraction osteotomy. Our goal was to measure and validate new angle to assess global kyphosis and to evaluate the sagittal balance after surgery. This is the first report which describes new angle to assess global kyphosis (T1-S1).
Materials and methods
Pre and postoperative controls were compared according to the Pelvic Incidence. The sagittal parameters ankylosing spondylitis patients were compared with 154 asymptomatic patients. In addition to the pelvic parameters and the C7 tilt, we used the spino-sacral angle.
Results
Pelvic incidence in ankylosing spondylitis patients was higher than asymptomatic population (61° vs. 51°). For a same tilt of C7 for both groups, the low pelvic incidence group had a lower sacral slope and pelvic tilt and a higher global kyphosis (spino-sacral angle = 90°) than the high pelvic incidence group (spino-sacral angle = 98°). In the adult volunteers, the C7 tilt and spino-sacral angle measured, respectively, 95° and 135°. The preoperative C7 tilt measured 73° and increased to 83° (p = 0.0025). The preoperative spino-sacral angle measured 96° and increased to 113.3° (p = 0.003).
Conclusion
A low pelvic incidence pelvis has a lower sacral slope than in high pelvic incidence and can support a bigger kyphosis. All the parameters were improved by the pedicle subtraction osteotomy, but the average spinosacral angle remained lower than the control group. When C7 tilt was useful to assess the improvement of the sagittal balance, SSA allowed a better evaluation of the correction of kyphosis itself.
Similar content being viewed by others
Introduction
Ankylosing spondylitis (AS) is an inflammatory arthritis that primarily affects the spine and sacroiliac joints [1]. Advanced stages of the disease are characterized by a progressive stiffening of the spine and thorax. The sagittal balance of the patient deteriorates during the course of the disease, producing a rigid thoracolumbar kyphosis. A severe thoracolumbar kyphosis results in a downward tilt of the head and face [2]. The ability of the patient to see above the level of the horizontal gaze progressively worsens. The center of gravity moves anteriorly, resulting in the stooped, downward looking posture that is characteristic of advanced AS. In an attempt to rectify this situation, the patient flexes the ankles and the knees, retroverts the pelvis positioning the hips in extension (when they seem to be clinically in flexion), and tilts the entire rigid segment of the spine backwards. This posture is usually unable to completely compensate for the thoracolumbar kyphosis. Therefore, the standing position of the patient represents the maximal posterior tilt of the pelvis, which is proved radiological by the orientation of sacral slope which may reach a complete horizontal orientation. This position is biomechanically inefficient, and painful, and the patient fatigues easily while walking or standing [3–8]. As hips are in maximal extension, there is a limited posterior gait step, increasing trunk forward imbalance when walking. The global position of the patient was evaluated by the C7 plumb line (Fig. 1); it should fall through the posterior superior corner of S1 and the hip joints. Legaye et al. [9] have described three angles that regulate spinal sagittal curves: pelvic incidence (PI), a shape pelvic parameter is the primary determinant of pelvic positioned parameters pelvic tilt (PT) and sacral slope (SS), due to the relation PI = PT + SS. PI is the adaptative parameter to correct worse spinal posture. The surgical management of this deformity is complicated, with controversies regarding different treatment approaches [3, 4, 10–14]. In general, the pathological posture of the spine and its correction by osteotomy has been evaluated by extrinsic parameters regarding vertical or horizontal lines. In this study, a new angle is used which described the intrinsic shape of the spine and pelvis.
The purpose of this current study was to describe new angles to assess global kyphosis regarding the pelvic shape and to evaluate the radiological outcomes of pedicle subtraction osteotomy in AS patients with severe fixed kyphotic deformity.
Materials and methods
Materials
The control group was a cohort of 154 asymptomatic young adult volunteers which were recruited mainly from the pool of medical and paramedical students at our institution. Results provided from previous published study [15].
The second group was composed by 28 consecutive AS patients with fixed kyphotic deformity underwent pedicle subtraction osteotomy (PSO) by the senior author. There were 9 females and 19 males with a mean age of 41.7 ± 8.3 years (range 22–64).
Radiologic assessment
A similar radiologic protocol was used at both situations, with 30 × 90 cm left-to-right lateral radiograph of the pelvis and entire spine obtained with each subject and patient. The distance from the radiographic source to the cassette was maintained at 230 cm for all exposures. The radiographic beam was centered with respect to the centroid of the rectangular cassette. Radiologic assessment was performed before operation and at last follow-up (minimum 2 years). In AS group knees were leaved in natural flexion for adaptative balance to the kyphosis. Sometimes due to the deformity, head could be outside the X-rays. But we always were able to capture C7-T1. In control group, lower limbs were always with knees in full extension.
Radiologic measurements included sacral slope (angle formed between the sacral endplate and the horizontal plane), pelvic tilt (angle between the vertical plane and a straight line joining the centers of the femoral heads and the center of the sacral endplate), pelvic incidence (angle between a line drawn from center of the hip axis to the center of the superior endplate of S1 and perpendicular to the endplate) and two new angles (Fig. 2a). The L line was definite by the line joining the center of C7 and the center of the sacral endplate). The first was the C7 tilt (C7T) defined by the angle formed between the L line and the horizontal plane. The second was the spino-sacral angle (SSA); it was the angle between the L line and the sacral endplate. SSA was intrinsic angles of the spine and pelvis. In a rigid spine, they were considered as shape angles, when C7tilt was an extrinsic and positional angle.
The both cohorts were measured with dedicated software (Softimage Spine, Optimage, Lyon, France) on numerical X-rays. Statistical analysis was done by Wilcoxon signed ranks test and paired sample t test.
Operative methods
The current authors performed osteotomy at L4 in the early stage of this study (Fig. 2b). One-level osteotomy was performed in all patients. Osteotomies were performed at L3 in 12 and L4 in 16 patients. Angulations osteotomies ranged between 30° and 40°.
Results
In the young adult volunteers, the mean ± standard deviation C7 tilt, and SSA measured, respectively, 95.4° ± 1.4°, 135.2° ± 3.8°.
In AS patients with fixed kyphotic deformity whose underwent pedicle subtraction osteotomy the changes of various angles figure in Table 1. The mean preoperative C7 tilt measured 72.6° ± 14.7° and increased to 83.1° ± 7.3° at the final follow-up (p = 0.0025). The mean preoperative SSA measured 96.4° ± 17.8° and increased to 113.3° ± 11.6° at the final follow-up (p = 0.003).
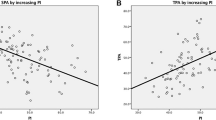
The pelvic incidence (PI) measured 50.6 ± 5.2° in the control group and 61.9 ± 13.7 in SA group. The patients with a low PI (PI ≤ 50°, n = 7) had a lower preoperative SSA compared to the patients with a high PI (PI > 50°, n = 21). The preoperative C7 tilt were similar in theses both groups. The radiological details of the AS patients in function of the PI were resumed into Tables 2 and 3 and exposed into Fig. 3.
Radiological results of the AS patients in function of the PI value. SS pre sacral slope preoperative, SS post sacral slope postoperative, PI pelvic incidence, SSA pre spino-sacral angle preoperative, SSA post spino-sacral angle postoperative, C7T pre C7 tilt preoperative, C7T post C7 tilt postoperative
Discussion
Radiological assessment
Several authors have demonstrated that the radiographic appearance of kyphosis is dependent upon the position of the lower extremities [5, 6]. It is not possible to measure the position of the lower extremities on the same lateral radiograph as the spine and pelvis. Therefore, it is important to describe the relationship between the pelvis and the spine in a way that is independent of the position of the hips, knees and ankles. The spino-pelvic angle (SPA) is defined as the angle between a line from the center of C7 to the center of the sacral endplate and a line from the center of the sacral endplate to the center of the hip axis. In a presence of a kyphotic deformity, the angle decreases significantly. The SSA is defined as the angle between a line from the center of C7 to the center of the sacral endplate and the sacral endplate itself. SSA is correlated at the kyphosis. It may be useful in the strategy correction. In our series PI is significantly increased compared to our control group. All our patients were operated for severe kyphosis. Two explications are possible: either the high PI patients are less able to compensate, either a flat back with a low PI is less able to develop a severe kyphosis by the way of the disease (flat remains flat, high lordosis may decrease).
Adaptation of the sagittal balance in evolution of a kyphotic deformity
The stages of adaptation to a significant kyphosis with anterior displacement of the center of gravity proceeds as follows; in order to maintain C7/T1 over the endplate of the sacrum, pelvic tilt is first increased by extension of the hips, and once amount of pelvic tilt reaches the maximum, the knees are flexed in order to tilt the rigid spine and pelvis posteriorly.
When the patient tilts the pelvis posteriorly, the sacral end offset regarding femoral heads increases. On a geometrical point of view, as the sum of the sacral slope and the pelvic tilt is equal to pelvic incidence, the ability of the spine to compensate for the deformity is limited by the patient’s native anatomic alignment. A patient with a large pelvic incidence is able to compensate for a kyphotic deformity by inducing a large posterior tilt to the pelvis, until reaching a flat sacral endplate, this increases the sacral end offset. However, a patient with a very low pelvic incidence does not have the same capacity to accommodate the deformity. In of others terms, to a same quantity of kyphosis (C7tilt), a patient with a high pelvic incidence will have a higher SSA than a patient with a low pelvic incidence.
Theoretically a patient with a low PI would be less able to compensate a severe kyphosis than one with high PI. As the maximum retroversion provided by a low PI pelvis is inferior to a high PI, when SS trends to 0°. In our study we do not confirm this evidence. SSA is bigger in low PI patients than in high PI. On another way the average SS is closer to horizontal in low PI than in high PI. According to C7 position the level of imbalance is the same in all cases. It seems that in low PI it is easier to reach a 0° of SS than in high PI. This is probably due to the limitation of hips extension which forbid on the pelvis to reach a too high level of retroversion.
Effect of lumbar osteotomy for kyphosis correction
The severity of the kyphosis and the results of surgical treatment are well assessed by the SSA which may be considered as an evaluation of the whole kyphosis of both thoracic and lumbar area. The comparison with the asymptomatic population shows that the SSA is lower than 39° in the ankylosing spondylitis patients. After surgical treatment, it is improved by only 17°. As kyphosis is not corrected enough, they are still compensation in pelvic position (increasing retroversion). The sagittal balance is not sufficiently corrected with a low sacral slope (30°) and a high pelvic tilt (31°). The position of C7 characterized by the C7 tilt was largely anterior before surgery (72° for a normal at 95°) and better positioned after (83°).
The goals of surgical correction of sagittal malalignment in ankylosing spondylitis are to decrease the cosmetic and functional effects of the deformity, reduce the patient’s pain and increase their ability to stand and walk comfortably [4, 7, 16, 17]. A number of techniques for inducing a posterior tilt to the spine and returning the gaze to the horizontal have been described [3, 11, 17–20]. These techniques include an opening wedge anterior osteotomy, vertebral body corporectomy and realignment, multiple posterior wedge osteotomies of the posterior elements only, and osteotomy of the anterior and posterior column or pedicle subtraction technique.
In the process of preoperative planning, it is important to determine both how much correction is desirable, and how much correction is achievable. In the published results with pedicle subtraction, single level corrections of more than 40° are rare [4, 17]. If more than 40° of correction is desirable, then multiple closing wedges of the spine are likely to be necessary.
The amount of correction that is needed to place the center of C7 vertebral body directly above the sacral endplate with the patient’s knees in extension is determined by the amount of kyphosis and the alignment of the spine and pelvis. Our results demonstrate that when both groups high and low PI, preoperative C7 tilt was similar after surgery there were a better position of C7 in low PI group. The global balance was better in the low PI group ever with a worse SSA initial angle. Our results suggested that with only one level of PSO, the ideal balance was not achieved (SSA close to 135°, pelvis tilt around 20°) in all our patients and worse in those with a high grade PI.
In summary, there is an important difference between balances of severe kyphosis regarding the value of Pelvic Incidence. In case of low pelvic Incidence, SSA has to be higher than in a system with a high PI to position C7 with a same plumb line with regard to the pelvis. In other words to have the same C7 plumb line position, there is more kyphosis deformity with High PI pelvis than with low PI pelvis (Fig. 4). The strategy of correction has to take in account both the repositioning of C7 plumb line and the reduction of the pelvis tilt. We propose a geometrical sequence of calculation of the quantity of SPO using the correction of SSA. The first step is to rotate the whole set of spine and pelvis around the femoral head axis in order to bring the sacral end with an average ideal Pelvis Tilt of 20°. Then in a second step we virtually bring C7 over the pelvis. This maneuver provides the quantity of correction of SSA necessary to perform an ideal osteotomy. Evidently this strategy is useful only in case of rigidity of the whole spine like in SA diseases. It is evident on Fig. 5a, b that the correction of a same unbalanced C7 plumb line needs a smaller osteotomy in case of low grade incidence than with a high Pelvic Incidence. The strategy of correction of severe kyphosis has to take in account the level of pelvic incidence to appreciate the quantity of the osteotomy.
Conclusion
Pedicle subtraction osteotomy in ankylosing spondylitis patients with severe fixed kyphotic deformity was safe and could obtain the large amount of correction with a single-level osteotomy. Postoperatively, all the parameters were improved by the PSO but the average SSA remained lower than the control group mainly when there was a high grade pelvic incidence. SSA is a good indicator to assess the whole deformity of the spine in severe kyphosis. Its insufficient correction by a PSO alone explains the remaining retroverted pelvis after correction. When C7 tilt was useful to assess the improvement of the balance, SSA allowed a better evaluation of the correction of kyphosis itself. We must emphasize the role of the pelvic incidence in balancing severe kyphosis and in strategy of correction by PSO.
References
McMaster MJ, Coventry MB (1973) Spinal osteotomy in ankylosing spondylitis. Technique, complications, and long-term results. Mayo Clin Proc 48:476–486
White AA 3rd, Panjabi MM, Thomas CL (1977) The clinical biomechanics of kyphotic deformities. Clin Orthop Relat Res 128:8–17
Berven SH, Deviren V, Smith JA et al (2001) Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine 26:2036–2043
Kim KT, Suk KS, Cho YJ et al (2002) Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine 27:612–618
Van Royen BJ, De Gast A, Smit TH (2000) Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J 9:492–498
Van Royen BJ, Toussaint HM, Kingma I et al (1998) Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Eur Spine J 7:408–412
Camargo FP, Cordeiro EN, Napoli MM (1986) Corrective osteotomy of the spine in ankylosing spondylitis. Experience with 66 cases. Clin Orthop Relat Res 208:157–167
Suk KS, Kim KT, Lee SH et al (2003) Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine 28:2001–2005
Legaye J, Duval-Beaupere G, Hecquet J et al (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Bridwell KH, Lewis SJ, Lenke LG et al (2003) Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am 85-A:454–463
Hehne HJ, Zielke K, Bohm H (1990) Polysegmental lumbar osteotomies and transpedicled fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis. Report on 177 cases. Clin Orthop Relat Res 258:49–55
McMaster MJ (1985) A technique for lumbar spinal osteotomy in ankylosing spondylitis. J Bone Joint Surg Br 67:204–210
Van Royen BJ, De Gast A (1999) Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment. Ann Rheum Dis 58:399–406
Van Royen BJ, Slot GH (1995) Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corporectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Br 77:117–121
Roussouly P, Gollogly S, Noseda O et al (2006) The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine 31:E320–E325
Chen PQ (1988) Correction of kyphotic deformity in ankylosing spondylitis using multiple spinal osteotomy and Zielke’s VDS instruments. Taiwan yi xue hui za zhi 87:692–699
Bridwell KH, Lewis SJ, Edwards C et al (2003) Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine 28:2093–2101
Van Royen BJ (2002) A new technique for correction of an iatrogenic extension deformity in ankylosing spondylitis. Spine 27:332–333
Van Loon PJ, Van Stralen G, Van Loon CJ et al (2006) A pedicle subtraction osteotomy as an adjunctive tool in the surgical treatment of a rigid thoracolumbar hyperkyphosis; a preliminary report. Spine J 6:195–200
Noun Z, Lapresle P, Missenard G (2001) Posterior lumbar osteotomy for flat back in adults. J Spinal Dis 14:311–316
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
R. Debarge, G. Demey, P. Roussouly: Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur Spine J (2010) 19: 65–70. © Springer-Verlag 2009. With permission of Springer Science + Business Media.
Rights and permissions
About this article
Cite this article
Debarge, R., Demey, G. & Roussouly, P. Sagittal balance analysis after pedicle subtraction osteotomy in ankylosing spondylitis. Eur Spine J 20 (Suppl 5), 619 (2011). https://doi.org/10.1007/s00586-011-1929-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-011-1929-9