Abstract
Previous cadaveric studies have suggested that forefoot deformities at the metatarsophalangeal (MTP) joints in patients with rheumatoid arthritis (RA) might result from the failure of the ligamentous system and displacement of the plantar plates. This study aimed to examine the relationship between plantar plate pathology and the rheumatoid arthritis magnetic resonance imaging score (RAMRIS) of the lesser (second to fifth) MTP joints in patients with RA using high-resolution 3 T magnetic resonance imaging (MRI). In 24 patients with RA, the forefoot was imaged using 3 T MRI. Proton density fat-suppressed, T2-weighted fat-suppressed and T1-weighted post gadolinium sequences were acquired through 96 lesser MTP joints. Images were scored for synovitis, bone marrow oedema and bone erosion using the RAMRIS system and the plantar plates were assessed for pathology. Seventeen females and 7 males with a mean age of 55.5 years (range 37–71) and disease duration of 10.6 years (range 0.6–36) took part in the study. Plantar plate pathology was most frequently demonstrated on MRI at the fifth MTP joint. An association was demonstrated between plantar plate pathology and RAMRIS-reported synovitis, bone marrow oedema and bone erosion at the fourth and fifth MTP joints. In patients with RA, 3 T MRI demonstrates that plantar plate pathology at the lesser MTP joints is associated with features of disease severity. Plantar plate pathology is more common at the fourth and fifth MTP joints in subjects with RA in contrast to the predilection for the second MTP reported previously in subjects without RA.
Similar content being viewed by others
Introduction
The foot is commonly involved in rheumatoid arthritis (RA), particularly at the metatarsophalangeal (MTP) joints [1, 2]. On magnetic resonance imaging (MRI) synovitis, erosion and bone oedema are well recognised in the foot but the plantar plate is seldom routinely visualised. In RA the function of the plantar plate in forefoot deformity is poorly understood.
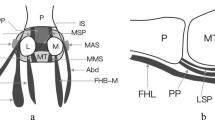
The plantar plate (Fig. 1) is the major distal attachment of the plantar fascia, inserting into the proximal phalanx. Proximally it attaches to the metatarsal shaft with the two collateral ligaments providing the most substantial attachment of the plantar plate to the metatarsal. The flexor tendon sheath, which encompasses the flexor digitorum longus and brevis tendons lies immediately plantar to the plantar plate and is adherent to the outer borders of the plantar surface of the plate. The plate is a fibrocartilaginous structure which together with the deep transverse metatarsal ligament has an important role in maintaining the structural integrity of the MTP joints [3]. During walking, the forces imposed as the toes push off cause repeated hyperextension of the MTP joint, and it has been postulated that this may predispose the plantar plates to attenuation or rupture [3]. Degeneration or loss of function of the plantar plate is a potential mechanism through which the characteristic forefoot deformity may develop in patients with RA.
a Sagittal illustration through the lesser MTP joint, the plantar plate (short arrow) inserts into the proximal phalanx (P) and the flexor tendon (long arrow) lies adjacent to the plantar plate. b Short axis illustration through the forefoot, proximally the plantar plate (PP) attaches to the metatarsal shaft (MT) with the two collateral ligaments (CL) providing the most substantial attachment of the plantar plate to the metatarsal. The dorsal interosseous tendon (I) with the accessory CL insert into the dorsal aspect of the plantar plate. The flexor tendon sheath (FT) lies immediately plantar to the plantar plate and the deep transverse metatarsal ligament (TML) runs between the metatarsals attaching to the plantar plates
Cadaveric studies of the feet in RA have suggested that forefoot deformities in RA might result from failure of the complex ligamentous system and the dynamic effect of displacement of the plantar plates [4]. However, the structures involved, the potential mechanisms by which changes occur and the relationship between synovial, bone and plantar plate abnormalities have not been clearly identified in patients with RA.
MRI has been used to identify the plantar plate and visualise tears in normal subjects [5] but has not been used at high field strengths to image the plantar plate in patients with RA. The rheumatoid arthritis magnetic resonance imaging score (RAMRIS) allows semiquantative, standardised assessment of inflammatory and destructive changes in RA [6, 7] and has excellent interreader and intrareader reliability in the assessment of the forefoot (MTP joints) in patients with RA [8]. Furthermore the relationship between plantar plate pathology, synovitis and bone change in patients with RA has not been reported previously. The aim of this study was to use MRI to investigate the relationship between plantar plate pathology and RAMRIS in the lesser (second to fifth) MTP joints in patients with RA.
Materials and methods
Recruitment of patients
Local ethical approval was received and written consent obtained from all participants. Consecutive patients diagnosed with RA, according to the 1987 American College of Rheumatology revised criteria for RA [9] (data were acquired prior to 2010 rheumatoid arthritis classification criteria [10]), and presenting to a specialist rheumatology foot clinic were invited to take part in the study. Patients were recruited between August and December 2009. The first MTP joint was not studied because of the different anatomy and pattern of pathological changes compared to the lesser MTP joints. Patients were excluded if they had a diagnosis of diabetes, peripheral vascular disease, peripheral neuropathy, a history of forefoot surgery or contraindications to having a MRI scan or intravenous contrast.
Clinical measures
Demographic data and current medication were recorded for each patient. In order to quantify current disease activity, a disease activity score (DAS 44) which includes the MTP joints was used. A tender and swollen joint count was performed by an experienced research nurse (DAP) and inflammatory markers (C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)) were obtained in order to establish a current disease activity score (DAS 44 (CRP) and DAS 44 (ESR)). Platto’s Structural Index was completed to assess the forefoot structural deformity present [11], the index score includes the presence or absence of hallux valgus and fifth MTP joint exostosis, and the number of cock/hammer/claw toes present (0–5) and subluxed MTP joints (0–5).
MRI protocol
The forefoot was imaged using a 3-T Verio scanner (Siemens Healthcare, Erlangen, Germany) with an extremity radio frequency coil. Intermediate-weighted fat-suppressed sagittal (Fast spin echo, repetition time (TR) = 3,500 ms, echo time (TE) = 35–61 ms, 0.5 × 0.3 mm in-plane resolution, 3 mm slice thickness) and T2-weighted fat-suppressed short and long axis images (Fast spin echo, TR = 3,100–4,300 ms, TE = 85–92 ms, 0.5 × 0.3–0.4 mm in-plane resolution, 3 mm slice thickness) were acquired through the lesser MTP joints. 3D VIBE post contrast images (TR = 9 ms, TE = 5 ms, flip-angle = 30 degrees, 0.7 × 0.6 × 0.6 mm resolution) were acquired after the administration of 0.1 mmol/kg intravenous contrast agent (Gd-DOTA, Guerbert, France) together with pre and post contrast T1 weighted fat-supressed images (spin-echo, TR = 900 ms, TE = 16ms, 0.5 × 0.3 mm in-plane resolution) if the patient was able to tolerate further time in the scanner.
Images were scored for synovitis (0–3), bone marrow oedema (0–3) and bone erosion (0–10) at each lesser MTP joint, respectively (Fig. 2), using the RAMRIS defined by the outcome measures in rheumatoid arthritis clinical trials group [6–8]. RAMRIS has demonstrated excellent reliability in assessment of the forefoot in patients with RA [8]. Plantar plate pathology (Figs. 3 and 4) was defined from sagittal and axial MR images as the absence of (failure to visualise) the plantar plate, or a full-width or partial-width tear, including failure to visualise the medial or lateral distal insertions. MR images were read by two experienced musculoskeletal radiologists (RJH and AJG) and consensus was reached.
Images through the MTP joints of a patient with RA showing synovitis, bone marrow oedema and bone erosion. a Long axis T2-weighted fat-suppressed image showing extensive bone marrow oedema (white arrows). b Sagittal post contrast T1-weighted image showing synovitis (black arrow). The plantar plate is absent and synovitis extends from the joint to the flexor tendon. c Long axis and d short axis reconstructions from T1-weighted post contrast 3D VIBE images, again showing synovitis (black arrows) and erosion of the metatarsal heads (black arrowheads)
a Sagittal intermediate-weighted and b short axis T1-weighted fat suppressed images through the second MTP joint of a patient with RA showing an intact plantar plate (arrow), deep to the flexor tendon (long arrow). Small amount of high signal is seen at the insertion of the plantar plate into the proximal phalanx centrally (arrowhead), a common finding. (Cystic change is noted in first metatarsal head). c Sagittal intermediate-weighted and d short axis T2-weighted fat-suppressed images through the second MTP joint of a patient with RA. There is dislocation of the joint and the plantar plate is not visualised. There is bone marrow oedema (open arrow). On short axis section, fluid can be seen tracking from the joint around the flexor tendon sheath (arrow)
a and b (adjacent slices) Sagittal intermediate-weighted, c short axis T2-weighted fat-suppressed and d short axis T1 fat suppressed images through the second MTP joint demonstrating a tear (between arrowheads) of the plantar plate (arrow). The flexor tendon (long arrow) is adjacent to the bone distally without interposed plantar plate. There is extensive bone marrow oedema (open arrow)
Statistical methods
In order to identify associations between RAMRIS and the odds of plantar plate pathology at the lesser MTP joints in patients with RA, proximal and distal bone oedema scores and proximal and distal bone erosion scores were summated to give a total bone oedema score and a total bone erosion score per lesser MTP joint. These were then coded into three score categories (0, 1 and >2). Comparison of a multilevel model containing only plantar plate pathology status and controlling for clustering at the patient level with a single-level model that did not control for clustering gave some indication that substantive cluster effects were present, given that the sample size was small and the likelihood ratio test is conservative (chi-bar = 2.07, p = 0.075). Therefore, multilevel modelling was used to explore the association between RAMRIS and the odds of plantar plate pathology. Multilevel binary logistic regression models were constructed in which plantar plate pathology was the outcome and either the synovitis, bone oedema or bone oedema score was the primary predictor at the joint level. Odds ratios were also calculated for the third to fifth MTP joints relative to the second MTP joint. The forefoot Platto Structural Index score was included as a patient (foot)-level contextual factor.
Results
Demographic and disease characteristics
Twenty-seven patients were approached to take part in the study; 24 patients with RA (17 females and 7 males) met the inclusion criteria and took part in the study. Patients’ mean (SD) age was 55.5 (10.5) (range 37–71) years and disease duration was 10.6 (8.6) (range 0.6–36) years. Eighteen patients were rheumatoid factor positive, the mean (SD) DAS44 (CRP) and DAS44 (ESR) were 2.5 (0.8) and 2.6 (0.9), respectively. Twenty-three patients were taking a disease modifying anti-rheumatic drug, 15 patients (63%) were taking a biologic therapy and 1 patient was taking oral steroids. The median (range) forefoot Platto Structural Index score was 8.0 (2–12). There was some evidence that MTP joints from feet with a forefoot Platto Structural Index scores above the median of the distribution (>8) were more likely to show plantar plate pathology [24/48 (50.0%)] than those from feet with lower scores [14/48 (29.2%)]. Platto index (≤8, >8) was therefore included in each multilevel model as a level 2 contextual factor. No statistically significant associations were found between forefoot Platto Structural Index score and plantar plate pathology.
Plantar plate pathology seen on MRI
At the patient level, one or more lesser plantar plates were absent in nine (38%) patients. All the lesser plantar plates were absent in one patient. Tears in one or more lesser plantar plates were identified in 14 (58%) patients.
At the joint level, 16/96 (17%) plantar plates were absent and tears were observed in 22 (28%) of the 80 remaining plantar plates. All tears were located distally in the plantar plates. Five (23%) were full-width tears and the majority (94%) of partial tears were situated on the medial aspect of the plantar plate.
Table 1 shows the number of patients with plantar plate, bone and synovial pathology at each lesser MTP joint. The fifth MTP joint was the most common site for all types of pathology. The associations between plantar plate pathology and features of RA disease at each lesser MTP joint are given in Table 2.
RAMRIS synovitis and plantar plate pathology
No substantive or statistically significant interactions were found between the RAMRIS synovitis categories and the four lesser MTP joints, indicating that the association between plantar plate pathology and RAMRIS synovitis score category was consistent across the four lesser MTP joints (and vice versa). Plantar plate pathology was more prevalent in the fourth MTP joint [OR = 9.44 (1.55 to 57.53), p = 0.015] and fifth MTP joint [OR = 32.70 (4.31 to 248.190), p = 0.001] relative to the second MTP joint but the third MTP joint did not significantly differ from the second MTP joint [OR = 1.72 (0.30 to. 9.77), p = 0.538]. The odds of plantar plate pathology were increased in joints with synovitis grade 2 or above relative to those where synovitis was absent [OR = 15.52 (1.01 to 238.54), p = 0.049] but odds for joints with grade 1 synovitis did not differ to a statistically significant degree [OR = 6.07 (0.72 to 51.12), p = 0.097]. The model as a whole was significantly better than the null model (Wald chi-square = 15.18, p = 0.019).
RAMRIS bone oedema and plantar plate pathology
No substantive or statistically significant interactions were found between MTP joint and the RAMRIS bone oedema categories and the four lesser MTP joints, indicating that the differences in prevalence of plantar plate pathology across the MTP joints were consistent. It also indicated that the association between plantar plate pathology and RAMRIS bone oedema score category was consistent across the four lesser MTP joints (and vice versa). Within any given bone oedema score, plantar plate pathology was more prevalent at the fourth MTP joint [OR = 11.32 (1.57 to 81.74), p = 0.016] and the fifth MTP joint [OR = 44.26 (3.96 to 494.01), p = 0.002] compared to the second MTP joint. However, plantar plate pathology was not significantly more prevalent at the third MTP joint [OR = 2.47 (0.40 to 15.41), p = 0.332]. In any given lesser MTP joints, odds of plantar plate pathology were increased in joints with bone oedema score of 2 or above [OR = 9.86 (1.61 to 60.40), p = 0.013] relative to those where bone oedema was absent (score 0). MTP joints with a score of 1 did not differ significantly [OR = 2.04 (0.30 to 13.98), p = 0.469]. The model as a whole was significantly better than the null model (Wald Chi-square = 14.07, p = 0.029).
RAMRIS bone erosion and plantar plate pathology
No substantive or statistically significant interactions were found between MTP joint and the RAMRIS erosion categories. At any given erosion category, plantar plate pathology was more prevalent at the fourth MTP joint [OR = 24.74 (2.21 to 277.33), p = 0.009] and fifth MTP joint [OR = 85.63 (4.84 to 1515.97), p = 0.002] compared to the second MTP joint. However, plantar plate pathology was not significantly more prevalent at the third MTP joint [OR = 1.75 (0.25 to 12.15), p = 0.572]. Odds of plantar plate pathology were increased in joints with an erosion score of 1 [OR = 13.76 (1.18 to 160.98), p = 0.037] or 2 or more [OR = 91.53 (6.19 to 1354.25), p = 0.001] relative to those where erosions absent (score 0). The model as a whole performed significantly better than the null model (Wald chi-square = 13.02, p = 0.043).
Discussion
This is the first exploratory study to use MRI to investigate plantar plate pathology at the lesser MTP joints in patients with RA. The study has demonstrated that plantar plate pathology is common in RA and provides evidence for an association with synovitis, bone oedema and bone erosion at the lesser MTP joints.
Patients with RA and RAMRIS-reported synovitis, bone oedema and bone erosion were more likely to have plantar plate pathology present at the fourth and fifth MTP joints compared to the second MTP joint. This is supported by the frequency of plantar plate pathology seen at the fifth MTP joint, known to be the commonest site of erosive change in the forefoot [12–14]. The current findings are in contrast to previous studies of plantar plates of healthy subjects in which plantar plate tears have been reported to most commonly occur at the second MTP joint, with significantly fewer being reported in the fifth plantar plate [15]. Furthermore, the odds of plantar plate pathology were increased in joints with synovitis and bone oedema score 2 or above and with erosions score 1 or greater, relative to those where RAMRIS scores were 0.
The plantar plate is a complex structure and in previous studies visualisation has been limited by the spatial resolution obtained [5]. This study used 3 T MRI with an optimised protocol and careful positioning of the MTP joints to allow better visualisation of the plantar plates and more sensitive differentiation of pathology [16].
In this cohort of patients with a relatively low disease activity (DAS 44 = 2.5), it appears that plantar plate pathology may be associated with current synovitis at the fourth and fifth MTP joints. However, only joints with a synovitis score of 2 or more had significantly higher odds of plantar plate pathology relative to joints without synovitis. This is not surprising as severity of synovitis may increase and decrease over time [17] while this study assesses synovitis at a single time point, providing no estimate of the average level of synovitis over time. This study suggests the possibility that plantar plate pathology could have been caused by higher levels of synovitis in the past, as has been suggested as a mechanism for bone erosion [18].
This study has not demonstrated an association between plantar plate pathology and forefoot deformity, measured using the forefoot Platto Structural Index. However, Platto’s Structural index incorporates deformity at the first MTP joint, which was excluded in the assessment of plantar plate pathology. Furthermore, the Platto Index is a clinician-reported, subjective measurement and therefore potential for error occurs, particularly in reporting of subluxation at the MTP joints.
The results of this study are limited by the relatively small sample size (n = 24) (and resulting large confidence intervals for the odds ratios). However, the patient demographics and disease characteristics are typical of this population of patients [19]. The small numbers in this study limited the ability to conduct a full multivariable analysis. As such it was not possible to evaluate whether RAMRIS-reported synovitis, bone oedema and bone erosion were related to plantar plate pathology independently of each other.
Plantar plate pathology appears common in this group of patients with RA presenting to a specialist rheumatology foot clinic (79.2% of patients), raising the possibility that plantar plate pathology may contribute to pain at the lesser MTP joints [4]. This study did not assess the relationship between forefoot pain and plantar plate pathology, and therefore further work is needed to establish whether there is a correlation between pain at individual MTP joints and plantar plate pathology at the same joint.
Although the results suggest an association between bone oedema and erosion and plantar plate pathology, no causative mechanism for this can be inferred from this cross-sectional study. It may be that altered biomechanics or mechanical effects due to plantar plate abnormalities cause bone changes such as oedema. Alternatively, bone irregularity due to erosion may lead to plantar plate tears. Another possible explanation could be the existence of a common cause for both bone and plantar plate pathology, such as past synovitis. Longitudinal follow-up studies of patients with RA and forefoot pain and deformity would help elucidate this. However, the current work will allow formal powering of larger studies to further investigate the role of the plantar plate in forefoot pain and disease progression in RA.
In conclusion, in this small exploratory study, plantar plate pathology appears to be associated with RAMRIS-reported synovitis, bone oedema and bone erosions at the lesser MTP joints of patients with RA. Plantar plate pathology was more common at the fourth and fifth MTP joints in people with RA, in contrast to the predilection for the second MTP reported previously in people without RA [15]. Refined MRI protocols allow for improved assessment of the progression of plantar plate pathology and should underpin future longitudinal studies.
References
Vidigal E, Jacoby RK, Dixon AS, Ratliff AH, Kirkup J (1975) The foot in chronic rheumatoid arthritis. Ann Rheum Dis 34(4):292–297
Grondal L, Tengstrand B, Nordmark B, Wretenberg P, Stark A (2008) The foot: still the most important reason for walking incapacity in rheumatoid arthritis: distribution of symptomatic joints in 1,000 RA patients. Acta Orthop 79(2):257–261
Johnston RB 3rd, Smith J, Daniels T, Johnston RB 3rd, Smith J, Daniels T (1994) The plantar plate of the lesser toes: an anatomical study in human cadavers. Foot Ankle Int 15(5):276–282
Stainsby GD (1997) Pathological anatomy and dynamic effect of the displaced plantar plate and the importance of the integrity of the plantar plate-deep transverse metatarsal ligament tie-bar. Ann R Coll Surg Engl 79(1):58–68
Yao L, Do HM, Cracchiolo A, Farahani K, Yao L, Do HM, Cracchiolo A, Farahani K (1994) Plantar plate of the foot: findings on conventional arthrography and MR imaging. AJR Am J Roentgenol 163(3):641–644
Ostergaard M, Peterfy C, Conaghan P, McQueen F, Bird P, Ejbjerg B, Shnier R, O’Connor P, Klarlund M, Emery P, Genant H, Lassere M, Edmonds J (2003) OMERACT rheumatoid arthritis magnetic resonance imaging studies. Core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. J Rheumatol 30:1385–1386
Ostergaard M, Edmonds J, McQueen F, Peterfy C, Lassere M, Ejbjerg B, Bird P, Emery P, Genant H, Conaghan P (2005) An introduction to the EULAR-OMERACT rheumatoid arthritis MRI reference image atlas. Ann Rheum Dis 64(Suppl 1):i3–i7
Baan H, Bezooijen R, Avenarius JK, Dubbeldam R, Drossaers-Bakker WK, van de Laar MA (2011) Magnetic resonance imaging of the rheumatic foot according to the RAMRIS system is reliable. J Rheumatol 38(6):1003–1008
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31(3):315–324
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JM, Hobbs K, Huizinga TW, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Menard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovsky J, Wolfe F, Hawker G (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 69(9):1580–1588
Platto MJ, O’Connell PG, Hicks JE, Gerber LH (1991) The relationship of pain and deformity of the rheumatoid foot to gait and an index of functional ambulation. J Rheumatol 18(1):38–43
Hulsmans HM, Jacobs JW, van der Heijde DM, van Albada-Kuipers GA, Schenk Y, Bijlsma JW (2000) The course of radiologic damage during the first six years of rheumatoid arthritis. Arthritis Rheum 43(9):1927–1940
Boutry N, Lardé A, Lapegue F, Solau-Gervais E, Flipo RM, Cotten A (2003) Magnetic resonance imaging appearance of the hands and feet in patients with early rheumatoid arthritis. J Rheumatol 30(4):671–679
van der Leeden M, Steultjens MP, Ursum J, Dahmen R, Roorda LD, Schaardenburg DV, Dekker J (2008) Prevalence and course of forefoot impairments and walking disability in the first eight years of rheumatoid arthritis. Arthritis Rheum 59(11):1596–1602
Gregg J, Silberstein M, Schneider T, Marks P (2006) Sonographic and MRI evaluation of the plantar plate: a prospective study. Eur Radiol 16(12):2661–2669
Siddle HJ, Redmond AC, Helliwell PS, Wakefield RJ, O’Connor PJ, Hodgson RJ (2010) High resolution MRI of asymptomatic plantar plate under flexion and extension: implications for understanding normal structure and diagnosing tears. Joint Annual Meeting ISMRM-ESMRMB 2010, Stockholm, Sweden
Verstappen SM, Poole AR, Ionescu M, King LE, Abrahamowicz M, Hofman DM, Bijlsma JW, Lafeber FP (2006) Radiographic joint damage in rheumatoid arthritis is associated with differences in cartilage turnover and can be predicted by serum biomarkers: an evaluation from 1 to 4 years after diagnosis. Arthritis Res Ther 8(1):R31
Jansen LM, van der Horst-Bruinsma IE, van Schaardenburg D, Bezemer PD, Dijkmans BA (2001) Predictors of radiographic joint damage in patients with early rheumatoid arthritis. Ann Rheum Dis 60(10):924–927
Symmons D, Turner G, Webb R, Asten P, Barrett E, Lunt M, Scott D, Silman A (2002) The prevalence of rheumatoid arthritis in the United Kingdom: new estimates for a new century. Rheumatology (Oxford) 41(7):793–800
Acknowledgments
The authors would like to thank Carole Burnett and Robert Evans from the NIHR Leeds Musculoskeletal Biomedical Research Unit for conducting the patient MRIs and William Davys for producing the illustrations in Fig. 1. HJS is funded by Arthritis Research UK (grant reference number 18007).
Disclosures
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Siddle, H.J., Hodgson, R.J., Redmond, A.C. et al. MRI identifies plantar plate pathology in the forefoot of patients with rheumatoid arthritis. Clin Rheumatol 31, 621–629 (2012). https://doi.org/10.1007/s10067-011-1899-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-011-1899-7